Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
What Causes Varicose Veins?
Varicose veins are visibly raised and swollen blood vessels beneath the surface of the skin. They are frequently seen on the lower legs, where they can be recognized by their blue, purple, or red coloration. Varicose veins are often a cosmetic concern, but they can also become itchy and painful. They are most common in women, older people, and those who are obese. Varicose veins are caused by a malfunction in the one-way valves in the veins that prevent blood from flowing backwards. Weakness or damage to the valves causes blood to pool in the veins. The pooled blood raises the venous pressure and makes the veins swell and twist. If you have varicose veins in your lower legs that are painful, it is suggested that you seek the care of a podiatrist for diagnosis and a treatment plan.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Fusion Foot and Ankle. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
When Gout Goes Untreated
Uric acid is produced as a by-product when the body breaks down purines contained in some of the foods we eat. When uric acid cannot be properly flushed, it can accumulate and crystalize on the joints: most commonly, the big toe joint. If this condition called gout goes untreated, nodules (tophi) can form which can be very painful and debilitating. In these cases where the disease has progressed or infection has set in (and more conservative treatments have not worked), surgery may be necessary. There are different surgical approaches to remove gouty deposits and tophic masses while preserving surrounding tissue. In extreme cases when the joint is severely damaged or unstable, joint replacement or fusion may be necessary to reduce pain. If you have episodes of sharp pain in the joint of the big toe, it is a good idea to make an appointment with a podiatrist to have your condition properly diagnosed and to explore your treatment options.
Gout is a painful condition that can be treated. If you are seeking treatment, contact one of our podiatrists from Fusion Foot and Ankle. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Are Bunions Affecting Your Everyday Life?
What Do Podiatrists Do?
Podiatrists are medical professionals who diagnose, treat, and offer preventative care for problems that affect the feet, ankles, and lower legs. Podiatrists may treat various foot and ankle injuries, such as plantar fasciitis, ankle sprains, and stress fractures. They can also address foot deformities, such as bunions, and skin or nail conditions like athlete’s foot or fungal toenails. A podiatrist might play a major role in a patient’s care if they have diabetes, poor circulation, or neuropathy, as these conditions frequently affect the feet. Some podiatrists are also trained in surgery. If you have developed a foot or ankle problem, it is suggested that you consult with a podiatrist.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact one of our podiatrists from Fusion Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
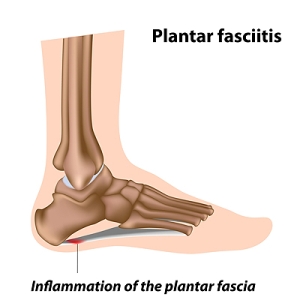
Plantar Fasciitis Prevention
 Plantar fasciitis is one of the most common foot injuries and the most frequent cause of heel pain. This condition occurs when the plantar fascia, a ligament that runs along the bottom of the foot, becomes inflamed usually due to repetitive stress and overuse. When the plantar fascia is injured, you may feel a sharp, stabbing pain in your heel and have pain in the arch of the foot. The pain is often at its worst when you take your first few steps in the morning or after a long rest. Fortunately, plantar fasciitis is both treatable and preventable. To prevent plantar fasciitis, it is suggested that you wear comfortable, well-fitted, supportive shoes, rest your feet after a workout or after standing for an extended amount of time, and stretch your feet regularly. If you are suffering from heel pain, don’t hesitate to schedule an appointment with a podiatrist near you.
Plantar fasciitis is one of the most common foot injuries and the most frequent cause of heel pain. This condition occurs when the plantar fascia, a ligament that runs along the bottom of the foot, becomes inflamed usually due to repetitive stress and overuse. When the plantar fascia is injured, you may feel a sharp, stabbing pain in your heel and have pain in the arch of the foot. The pain is often at its worst when you take your first few steps in the morning or after a long rest. Fortunately, plantar fasciitis is both treatable and preventable. To prevent plantar fasciitis, it is suggested that you wear comfortable, well-fitted, supportive shoes, rest your feet after a workout or after standing for an extended amount of time, and stretch your feet regularly. If you are suffering from heel pain, don’t hesitate to schedule an appointment with a podiatrist near you.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Fusion Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Fort Worth and Arlington, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.